This post picks up from a recent Facebook post about singing, stimming, and choosing my battles (actually, not choosing to battle), touching on what it means to accept preferred behaviours—mine and my son’s—and the power of being present. A recent Uniquely Human Podcast on Neuro-affirming care and PDA brought these thoughts into sharper focus, so I wanted to reflect more here.
Looking at the title now, it could just as easily be a DIY home improvement post—and in many ways, it is. It’s about the rewiring we do as parents when we’re raising children who don’t fit into neat boxes. A personal repair.
From Pathology to Autonomy
Although I dislike the terminology of PDA (Pathological Demand Avoidance), the discussion struck a chord with me, particularly in the linguistic and diagnostic origins. Dr. Taylor Day pointed out that PDA is still a theorised profile, and that it’s the idea rather than the label that often best reflects lived experience.
Reframed as a Persistent or Pervasive Drive for Autonomy, the description feels closer to the truth. It shifts the focus from disorder to understanding. From behaviour to the influencing context. It invites the question—not “what’s wrong with this behaviour?” but “what is influencing this reaction?”
It’s Not Defiance—It’s Survival
Dr. Day spoke about PDA as a nervous system response: a cascading stress that affects the entire family. Not one trigger, but many, layered, compounding causes. A build-up in a hypersensitive system that’s on alert, that is fight or flight, freeze, fawn, overwhelm, and shutdown. All combinations of which can result in a state of chronic stress, often invisible, increasing over time, for both parents and children. She proposes it stems from insecurity. From my personal point of view, it has been panicking and not knowing what to do. And when that happens, demands and triggers of any kind can feel like too much.
The idea that some of our kids are “super sensors” feels closer to the truth. These are children (and adults) who are exquisitely attuned to tone, emotion, and stress, often without the capacity to regulate or respond in ways that look typical. And when they can’t comply, they get labelled as manipulative or defiant. It’s heartbreaking. They’re not trying to control the situation. They’re trying to survive it.
Reframing, for us
Dr. Day invited us to rethink how we make demands, and why. A child’s “big reaction” might be the result of years of subtle (and not so subtle) pressures, often unknowingly passed down by us.
In the same podcast, Dr. Barry Prizant asked: Who should really be teaching us? It is so easy for professionals to assume their way is best. Their language, their diagnosis, their model. But shared human experience is essential. As human beings, we all come with our own lens. Our own wiring. Lived experience is no less valid than academia. Lived experience doesn’t need a PhD to be valid. It’s valid because it has been lived, a space and truth beyond textbooks. It was refreshing to hear that acknowledged. And that’s where conversations like this matter. It is the bridge to better understanding, improved approaches, and pivotal and pragmatic steps forward in DIY therapy and empowered parenting.
Repairing the system, too
Looking back, so much of the early support we received was compliance-focused. Sit still. Tick the boxes three times consecutively to pass for normal. But at what cost? With hindsight, my neurodivergence is something I understand better now. This isn’t about blame. It’s about a review. About asking: Why did I think that was the right path? What parts of me were just trying to survive, too? Neurodivergence, Autism, and related challenges don’t discriminate. They touch every class, background, and IQ level. It’s not about capacity. It’s about support. There is no hierarchy. And there’s no universal “right way”—only ways that work (or don’t) for each individual. It is a phenomenon that we continue to learn how to approach, theorise, and try out.
Letting Go of “Normal”
The repair work I’m doing now is more about shifting the focus away from neurotypical benchmarks—function, assessment, normalcy—and asking: What actually helps him?
So many therapeutic models still frame success as compliance. We need to ask—what’s actually serving our child? Not what makes others comfortable. Not what ticks boxes or looks good on paper.
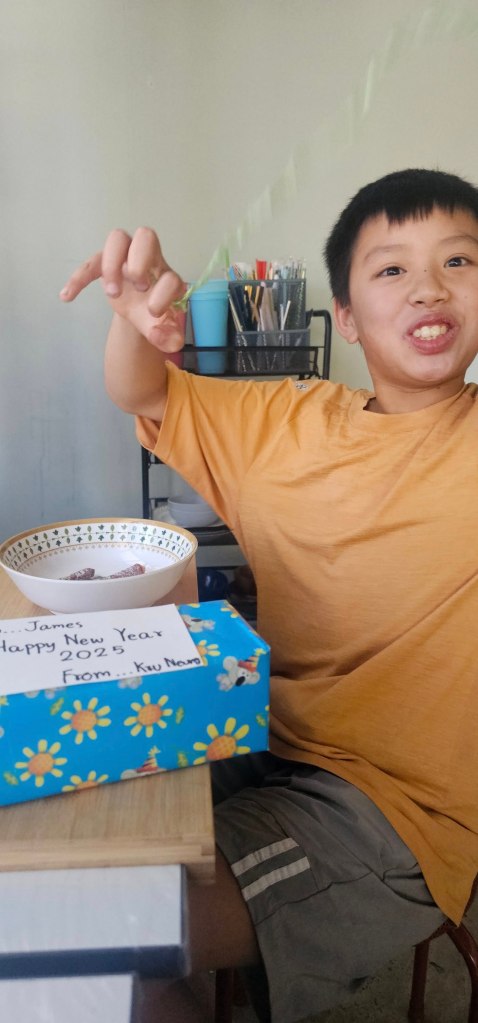
As my son enters the next phase of his life—physically the size of a man, on the edge of his teenage years—I think constantly about how the world can include him. He may need substantial support in daily life, but does that mean that life skills should be his priority? I’m more interested in developing his expression, communication, and preserving his youth. In nurturing self-advocacy. Of course, when safety isn’t the immediate concern.
He is where he is, in part, because of a larger inclusion problem. That’s why I keep doing this work: to keep changing how I see, how I respond, and how I show up for him.
Presence, Not Panic
One of the most powerful grounding tools Dr. Day shared was beautifully simple:
“Ask yourself, where are my feet right now?”
It’s so easy to live in the future as a parent, especially when your child’s future feels uncertain. What will happen when I’m gone? How will they cope? But anxiety steals the moment. And in the moment is where our children need us.
Instead of spiralling into all the unknowns, I try to focus on now. Enjoying our time together, and this sometimes means doing our own thing, but still checking in. Finding calm. This isn’t avoidance—it’s presence. And it’s powerful. It helps rewire my panic (neurological) pathways that have existed for a long time. It isn’t easy and it takes time, but the good news is that neuroplasticity can continue throughout our lives. Another leap of understanding in the field of neuroscience and neurobiology.
What really matters?
So instead of thinking in goals, guilt, outcomes, and “what should be,” I now try to think in contentment and connection. What helps my son feel safe? How can I support his autonomy? I turn to blogs, textbooks, and good news stories. And ultimately his behaviour tells me we are on the right track, for now.
Neurodivergent-affirming care starts with this:
- Seeing the person in front of you as whole and worthy.
- Understanding strengths and support needs, not just deficits.
- Prioritising quality of life over performance.
- Asking: Do they want to work on this? Not just: Do they need to?
This is respect and repair.
Not choosing battles—choosing peace
We hear a lot about “choosing our battles” in parenting. But maybe it’s time to step out of the battle altogether. If we see the stage our children are at, not as something to manage, but to meet with curiosity, then everything softens.
And it’s not just the child who needs care—we do too. Especially when neurodivergence runs in the family. Support needs to start with us, not end with us.
Uniquely Human Podcast
This podcast is full of insights—too many for me to cover here. I highly recommend listening to it. It’s one of those conversations that leaves you not with a checklist, but a shift in how you see things. And sometimes, that’s exactly what we need.